People are often nervous before surgery, so quitting smoking might be the last thing on their minds. Even thinking about quitting might be stressful. However, people who smoke frequently have complications after surgery, particularly with wound healing. It is essential that patients stop smoking before bariatric surgery.
What happens when you smoke…
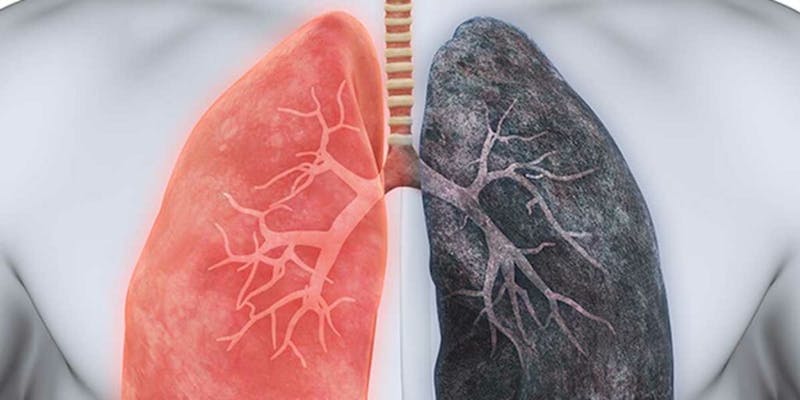
When you smoke, the amounts of carbon monoxide and nicotine in your blood increase. This reduces the amount of oxygen available that reaches the tissues throughout your body. Oxygen is essential to help wounds heal. Further, nicotine makes the heart work harder, partly because it increases blood pressure and pulse rate. Anesthetics and surgery also place a greater strain on circulation and oxygen supply, this might be worse for people who smoke.
Quitting smoking even only a short time before surgery could increase the amount of oxygen available in the body. Nicotine and the extra carbon monoxide from smoking start to disappear from the blood after 24 hours without cigarettes. Lung function starts to improve after about 2 months of quitting.
However, quitting smoking is difficult, especially in times of stress. One of the more common ways to try to quit is to use nicotine replacement therapy. This therapy helps reduce the withdrawal symptoms when you stop smoking. Nicotine replacement therapy may include a nicotine patch or nicotine chewing gum. There is less nicotine in replacement therapy than in cigarettes and, unlike cigarettes, nicotine replacement therapy does not increase the level of carbon monoxide in the body.
Researchers from The Cochrane Collaboration, an international network of researchers who work together to systematically analyze controlled trials.
Researchers found 8 trials involving almost 1,200 smokers. These people were having different kinds of surgery, including hip or knee replacement, breast surgery, bowel surgery or gynecological surgery. The trials did not cover all forms of surgery. Very few of these people were having heart surgery, and none were having lung surgery. However, there was still enough information on how smoking affects common complications, like problems with wound healing.
The strongest evidence about complications after surgery came from our experience at Obesity Control Center in Tijuana, Mexico. We encourage all our patients to stop smoking 4 weeks before surgery, and the complications rate drops dramatically. We also, performed pulmonary function test to evaluate the vital lung capacity, and from these results we start with incentive spirometer exercises.
We found two trials where people had weekly counseling sessions and nicotine replacement therapy starting at least 4 to 8 weeks before surgery, for them, the wound complications rate dropped from 28% down to 9%. In other words, out of every 100 people who use nicotine replacement therapy and are counseled before surgery, only 9 people can expect complications after surgery.
By comparison, out of every 100 people who do not have this counseling and therapy, 28 had complications. Some of the people who quit smoking before surgery were still not smoking months after the surgery, but some did resume their habits. Although it might still be possible to get benefits from quitting smoking closer to the date of surgery, the researchers concluded that it seems that at least four weeks might be necessary to reduce the risk of complications after surgery.

